What is Ependymoma?
Ependymoma is a tumor that arises from the ependyma, a tissue of the central nervous
system.
Usually, in pediatric cases the location isintracranial, while in adults it
is spinal. The common location
of intracranial ependymoma is the fourth ventricle. Rarely, ependymoma
can occur in the pelvic cavity.
Syringomyelia can be caused by an
ependymoma. Ependymomas are also seen with neurofibromatosis
type II.
These tumors are classified according to the presumed cell of origin. The most common types of cells in the nervous system are neurons and glial cells, although tumors from neurons are rare. Glial cells are the supportive cells of the brain and tumors arising from these cells are called gliomas. Subtypes of glial cells of the CNS include:
- Astrocytes cells
- Oligodendrocytes cells
- Ependymal cells
Diagnosis
A physician will perform a variety of diagnostic procedures to determine the exact type of tumor and whether the tumor has spread. These may include:
- physical exam - including neurologic function tests including: reflexes, muscle strength, eye and mouth movement, coordination and alertness.
- magnetic resonance imaging (MRI) - to produce detailed images of organs and structures within the body and/or spine
- computerized tomography scan (also called a CT or CAT scan) – used to capture
a detailed view of the body, in some cases
- biopsy – a tissue sample taken from the tumor during a
surgical procedure to provide information about the type of tumor
- lumbar puncture (also called an LP or spinal tap) - to remove a small sample of cerebrospinal fluid (CSF) and determine if any tumor cells have spread
 |
| MRI scan of Ependymoma of 4.ventricle |
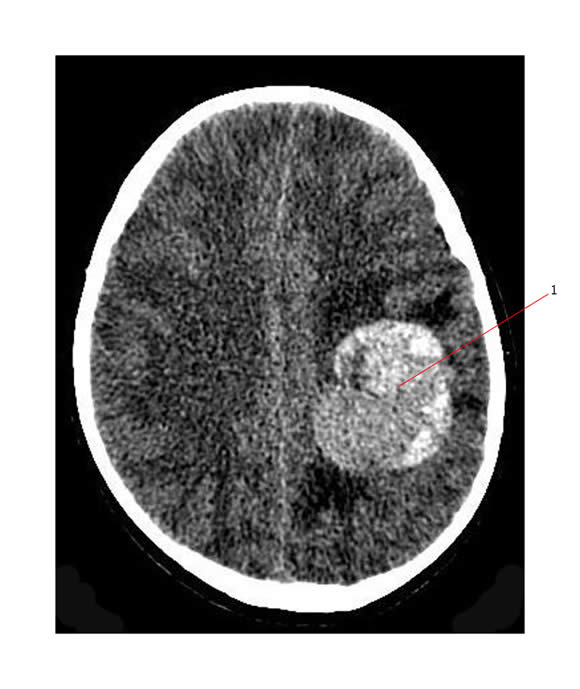 |
| CT scan showing a high grade supratentorial ependymoma in the left parietal region .
There is significant surrounding brain edema with mild midline shift.
|
Morphology
Ependymomas are composed of cells with regular, round to oval nuclei. There is a variably dense fibrillary background. Tumor cells may form gland-like round or elongated structures that resemble the embryologic ependymal canal, with long, delicate processes extending into the lumen; more frequently present are perivascular pseudorosettes in which tumor cells are arranged around vessels with an intervening zone consisting of thin ependymal processes directed toward the wall of the vessel.
It has been suggested that ependymomas are derived from radial glia.
Pathophysiology
 |
| Anaplastic epenymoma |
Anaplastic ependymoma is a type of malignant ependymomas tumor commonly found in young patients. These tumors grow rapidly and many people who develop them will experience complications or even die. This is especially true if the tumor is not caught and treated early. The majority of these growths, although rare, appear in children and adults that are younger than 25 years old. Tumors like this can appear in older adults, but are much more rare.
The diagnosis of an anaplastic ependymoma can sometimes be difficult because the symptoms associated with the tumor are also associated with other diseases and maladies.
Myxopapillary ependymoma (MEPN) is a slow-growing ependymoma (a type of glioma, which is a tumor that arises from the supportive tissue of the brain). They tend to occur in the lower part of the spinal column and are usually considered to be benign, low-grade or grade I tumors. The age of diagnosis ranges from 6 to 82 years.

Myxopapillary ependymomas are considered a distinct variant of ependymoma, occurring almost exclusively in the region of the cauda equina. These tumors are histologically characterized by elongated tumor cells arranged in a perivascular papillary pattern around central cores of mucinous or hyalinized perivascular stroma.
Subependymomas are nodular tumors composed of nests of ependymal cells in a dense glial fibrillary matrix. The majority of subependymomas are well delineated and arise as nodules in the fourth and lateral ventricles. They are thought to have a different, more benign prognosis than other types of ependymomas that occur in the brain.

The prognosis for a subependymoma is better than for most ependymal tumors, and is considered a grade I/IV tumor in the World Health Organization (WHO) classification.
This tumor forms from ependymal cells, and is a variation of an ependymoma.
Symptoms
·
Hydrocephalus
·
Increased
pressure inside skull
·
Headache
·
Papilloedema
·
Vomiting
·
Unsteadiness
·
Cognitive
problems
·
Behavioral
problems
·
Seizures
·
Nausea
·
Personality
changes
·
Vision
problems
·
Cranial nerve paresis
·
Impaired
memory
·
Speech
problems
·
Weakness
·
Motor
dysfunction
·
Dementia
·
Back pain
·
Numbness
·
Loss of bladder control
Grading of an Ependymoma
Grading refers to the appearance of the tumour cells under a microscope. The grade can give an idea of how quickly the tumour may develop. There are three grades of ependymoma. Grade 1 tumours are usually slow-growing and grade 3 tumours tend to grow more quickly.
The grades are:
- grade 1 - myxo-papillary ependymoma and sub-ependymoma
- grade 2 - ependymoma (low-grade)
- grade 3 - anaplastic (malignant) ependymoma.
Will they be able to survive?
PROGNOSIS: Extent of tumor resection and age of the patient are generally agreed upon as being predictive of outcome for children with ependymoma, but it is unclear whether tumor location or microscopic characteristics of the tumor are also prognostic indicators. The extent of surgical resection is the primary factor influencing survival, with a significantly better prognosis for patients with completely resected tumors. These patients with completely resected tumors have an estimated 5-year survival rate of 67-80%, compared to an estimated 5-year survival rate of 22-47% in patients with incompletely resected tumors. Most patients with incomplete tumor removal experience a tumor recurrence. Patients with residual tumor are also more than five times more likely to suffer from tumor spread through the cerebrospinal fluid.
Younger patients (< 4 years) have a worse prognosis, possibly due to a higher incidence of high-grade ependymomas, a more frequent lateral posterior fossa location of the tumor (which is more difficult to completely resect), or delays in initiating radiation therapy. Microscopic examination is unreliable in determining the long-term prognosis. In a study of almost 300 cases, the survival of patients with classic ependymoma was not markedly different from those patients with the anaplastic (high-grade) variant.
Treatment
Recommendations include:
·
Surgery
Here's a video of
Ependymoma of 4th Ventricle Surgical Removal
It describes the describes the surgical removal of a WHO Grade II ependymoma of the 4th ventricle including use of endoscopy.
·
Endoscopic
Third Ventriculostomy (ETV) or Ventriculo-peritoneal shunt (VP shunt) or brain
shunt
·
Radiation
therapy
·
Chemotherapy
References:
http://www.cern-foundation.org/Content.aspx?id=564
http://en.wikipedia.org/wiki/Ependymoma
http://www.childhoodbraintumor.org/brain-tumor-types-and-imaging/98-ependymomas.html
http://www.macmillan.org.uk/Cancerinformation/Cancertypes/Brain/Typesofbraintumours/Ependymoma.aspxhttp://www.wisegeek.com/what-is-a-anaplastic-ependymoma.htm

No comments:
Post a Comment